Is Over-Pronation
Overpronation and underpronation describe general foot movements. These terms do not necessarily describe a medical problem with a foot. For example, you can overpronate and not have any problems or symptoms at all. It is important to have your foot structure and symptoms adequately assessed by your prescribing physician and a qualified practitioner such as a Canadian Certified Pedorthist. Once the underlying conditions and mechanical faults are assessed, an appropriate treatment plan including possible orthotic and footwear recommendations can be made.
Causes
Over-pronation is very prominent in people who have flexible, flat feet. The framework of the foot begins to collapse, causing the foot to flatten and adding stress to other parts of the foot. As a result, over-pronation, often leads to Plantar Fasciitis, Heel Spurs, Metatarsalgia, Post-tib Tendonitis and/or Bunions. There are many causes of flat feet. Obesity, pregnancy or repetitive pounding on a hard surface can weaken the arch leading to over-pronation. Often people with flat feet do not experience discomfort immediately, and some never suffer from any discomfort at all. However, when symptoms develop and become painful, walking becomes awkward and causes increased strain on the feet and calves.
Symptoms
Eventually, over-pronation can lead to a full list of maladies including flat feet, plantar fasciitis, plantar fibroma, neuromas, heel spurs, shin splints, ankle sprains, bunions, hammertoes, calluses, and pain in the arches, knee, hip and lower back. But it doesn?t have to go that far, because there are steps we can take to correct the over-pronation. In the vast majority of cases, we?ll prescribe custom foot orthotics, which will realign your ankles, redistribute the weight, support the arch and reduce the twisting. Many orthotics will fit snugly into your normal shoes. Although we?ll also take a look at the type of shoes you wear to see if they are contributing to the problem.
Diagnosis
If you cannot afford to get a proper gait analysis completed, having someone observe you on a treadmill from behind will give you an idea if you are an overpronator. It is possible to tell without observing directly whether you are likely to be an overpronator by looking at your foot arches. Check your foot arch height by standing in water and then on a wet floor or piece of paper which will show your footprint. If your footprints show little to no narrowing in the middle, then you have flat feet or fallen arches. This makes it highly likely that you will overpronate to some degree when running. If you have low or fallen arches, you should get your gait checked to see how much you overpronate, and whether you need to take steps to reduce the level to which you overpronate. Another good test is to have a look at the wear pattern on an old pair of trainers. Overpronators will wear out the outside of the heel and the inside of the toe more quickly than other parts of the shoe. If the wear is quite even, you are likely to have a neutral running gait. Wear primarily down the outside edge means that you are a supinator. When you replace your running shoes you may benefit from shoes for overpronation. Motion control or stability running shoes are usually the best bet to deal with overpronation.

Non Surgical Treatment
Over-Pronation can be treated conservatively (non-surgical treatments) with over-the-counter orthotics. These orthotics should be designed with appropriate arch support and medial rearfoot posting to prevent the over-pronation. Footwear should also be examined to ensure there is a proper fit. Footwear with a firm heel counter is often recommended for extra support and stability. Improper fitting footwear can lead to additional problems of the foot. If the problem persists, call your doctor to schedule an appointment.
Surgical Treatment
Subtalar Arthroereisis. Primary benefit is that yje surgery is minimally invasive and fully reversible. the primary risk is a high chance of device displacement, generally not tolerated in adults.
An implant is pushed into the foot to block the excessive motion of the ankle bone. Generally only used in pediatric patients and in combination with other procedures, such as tendon lengthening. Reported removal rates vary from 38% - 100%, depending on manufacturer.
Severs Disease Facts And Figures
Sever?s disease, also referred to as calcaneal apophysitis, is an injury in the growth plate of the lower part of the heel bone where the Achilles tendon attaches to the bone. Sever?s disease is a common condition affecting children between the ages of 8 and 15 that participate in sports or are particularly active. This condition is believed to be caused by repeated trauma to the heel, weakening its internal structure. Typically occurring in adolescence, Sever?s disease causes painful inflammation of the growth plate. This condition can affect any child, however there is a higher probability of its occurrence if the child experiences pronation, has flat or high arches, short leg syndrome and/or is overweight.
Causes
With early puberty, the growth plate at the end of the heel develops, transforming cartilage cells into bone cells. This painful heel condition occurs during these growth spurts, when the heel bone grows more rapidly than the muscles and tendons of the leg. The discrepancy between rates of development causes excess pressure and tension to be placed upon the heel and it becomes less flexible. This condition affects active children the most. Due to the amount of exercise, more stress is placed upon the tendons which in turn causes more damage to the growth plate. The bone plates fully mature and harden by the time a child reaches the age of 15.
Symptoms
Activity-related pain that occurs on the back of the heel, where the Achilles tendon attaches on to the heel bone. Tenderness, pain & swelling on the heel bone. Difficulty walking or walking with a limp or on tiptoes.
Diagnosis
Sever?s disease can be diagnosed based on the symptoms your child has. Your child?s doctor will conduct a physical examination by squeezing different parts of your child?s foot to see if they cause any pain. An X-ray may be used to rule out other problems, such as a broken bone or fracture.
Non Surgical Treatment
Resting the foot and applying ice to the affected area are some of the most effective methods when it comes to treating Sever?s Disease. Make sure the ice is always wrapped in a cloth of some sort. Applying ice directly to the skin can cause frostbite. A monitored stretching program of the lower limbs (particularly of the calf muscles) as well as a small heel lift may also be suggested.
Exercise
The following exercises are commonly prescribed to patients with Severs disease. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 1 - 3 times daily and only provided they do not cause or increase symptoms. Your physiotherapist can advise when it is appropriate to begin the initial exercises and eventually progress to the intermediate, advanced and other exercises. As a general rule, addition of exercises or progression to more advanced exercises should take place provided there is no increase in symptoms. Calf Stretch with Towel. Begin this stretch in long sitting with your leg to be stretched in front of you. Your knee and back should be straight and a towel or rigid band placed around your foot as demonstrated. Using your foot, ankle and the towel, bring your toes towards your head as far as you can go without pain and provided you feel no more than a mild to moderate stretch in the back of your calf, Achilles tendon or leg. Hold for 5 seconds and repeat 10 times at a mild to moderate stretch provided the exercise is pain free. Calf Stretch with Towel. Begin this exercise with a resistance band around your foot and your foot and ankle held up towards your head. Slowly move your foot and ankle down against the resistance band as far as possible and comfortable without pain, tightening your calf muscle. Very slowly return back to the starting position. Repeat 10 - 20 times provided the exercise is pain free. Once you can perform 20 repetitions consistently without pain, the exercise can be progressed by gradually increasing the resistance of the band provided there is no increase in symptoms. Bridging. Begin this exercise lying on your back in the position demonstrated. Slowly lift your bottom pushing through your feet, until your knees, hips and shoulders are in a straight line. Tighten your bottom muscles (gluteals) as you do this. Hold for 2 seconds then slowly lower your bottom back down. Repeat 10 times provided the exercise is pain free.
What Is Posterior Tibial Tendon Dysfunction ?
Overview
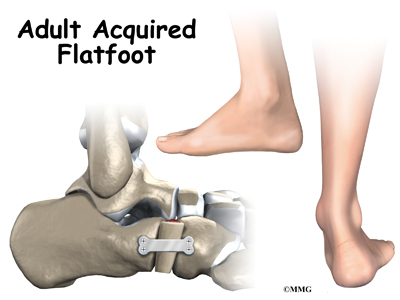
Adult acquired flatfoot is often a complex disorder, with diverse symptoms and varying degrees of deformity and disability. There are several types of flatfoot, all of which have one characteristic in common-partial or total collapse (loss) of the arch. Other characteristics shared by most types of flatfoot include ?Toe drift,? where the toes and front part of the foot point outward. The heel tilts toward the outside and the ankle appears to turn in. A short Achilles tendon or calf muscle, which causes the heel to lift off the ground earlier when walking and may act as a deforming force. In addition, other deformities such bunions and hammertoes can occur and cause pain in people with flexible flatfoot. Health problems such as rheumatoid arthritis, diabetes and obesity can increase the risk of developing flatfoot and may (or may not) make it more difficult to treat. This article provides a brief overview of the problems that can result in AAFD. Further details regarding the most common conditions that cause an acquired flatfoot and their treatment options are provided in separate articles. Links to those articles are provided. 
Causes
Posterior tibial tendon dysfunction is the most common cause of acquired adult flatfoot. Sometimes this can be a result of specific trauma, but usually the tendon becomes injured from wear and tear over time. This is more prevalent in individuals with an inherited flat foot but excessive weight, age, and level of activity are also contributing factors.
Symptoms
The symptom most often associated with AAF is PTTD, but it is important to see this only as a single step along a broader continuum. The most important function of the PT tendon is to work in synergy with the peroneus longus to stabilize the midtarsal joint (MTJ). When the PT muscle contracts and acts concentrically, it inverts the foot, thereby raising the medial arch. When stretched under tension, acting eccentrically, its function can be seen as a pronation retarder. The integrity of the PT tendon and muscle is crucial to the proper function of the foot, but it is far from the lone actor in maintaining the arch. There is a vital codependence on a host of other muscles and ligaments that when disrupted leads to an almost predictable loss in foot architecture and subsequent pathology.
Diagnosis
In diagnosing flatfoot, the foot & Ankle surgeon examines the foot and observes how it looks when you stand and sit. Weight bearing x-rays are used to determine the severity of the disorder. Advanced imaging, such as magnetic resonance imaging (MRI) and computed tomography (CAT or CT) scans may be used to assess different ligaments, tendons and joint/cartilage damage. The foot & Ankle Institute has three extremity MRI?s on site at our Des Plaines, Highland Park, and Lincoln Park locations. These extremity MRI?s only take about 30 minutes for the study and only requires the patient put their foot into a painless machine avoiding the uncomfortable Claustrophobia that some MRI devices create.
Non surgical Treatment
It is imperative that you seek treatment should you notice any symptoms of a falling arch or PTTD. Due to the progressive nature of this condition, your foot will have a much higher chance of staying strong and healthy with early treatment. When pain first appears, your doctor will evaluate your foot to confirm a flatfoot diagnosis and begin an appropriate treatment plan. This may involve rest, anti-inflammatory medications, shoe modifications, physical therapy, orthotics and a possible boot or brace. When treatment can be applied at the beginning, symptoms can most often be resolved without the need for surgery. 
Surgical Treatment
If conservative treatment fails to provide relief of pain and disability then surgery is considered. Numerous factors determine whether a patient is a surgical candidate. They include age, obesity, diabetes, vascular status, and the ability to be compliant with post-operative care. Surgery usually requires a prolonged period of nonweightbearing immobilization. Total recovery ranges from 3 months to one year. Clinical, x-ray, and MRI examination are all used to select the appropriate surgical procedure.
What Are The Leading Causes Of Adult Aquired Flat Foot ?
Adult Acquired Flatfoot occurs when the arch of your foot collapses after your skeleton has stopped growing, usually resulting in the foot falling inward with the toes pointing out. This allows your entire sole to touch the ground when you stand, instead of just the outside area. Arches fall for many reasons, including arthritis, injury to the supporting tendons or bones, nerve problems, diabetic collapse, pregnancy, aging, and obesity. A fallen arch doesn?t have to be painful-though as it develops and worsens, it can lead to strain and weakness in the feet that could allow for more uncomfortable foot problems later. Diabetics can develop serious complications from their fallen arches, and need to have their condition evaluated and treated.

Causes
As discussed above, many different problems can create a painful flatfoot. Damage to the posterior tibial tendon is the most common cause of AAFD. The posterior tibial tendon is one of the most important tendons of the leg. It starts at a muscle in the calf, travels down the inside of the lower leg and attaches to the bones on the inside of the foot. The main function of this tendon is to support the arch of your foot when you walk. If the tendon becomes inflamed or torn, the arch will slowly collapse. Women and people over 40 are more likely to develop problems with the posterior tibial tendon. Other risk factors include obesity, diabetes, and hypertension. Having flat feet since childhood increases the risk of developing a tear in the posterior tibial tendon. In addition, people who are involved in high impact sports, such as basketball, tennis, or soccer, may have tears of the tendon from repetitive use. Inflammatory arthritis, such as rheumatoid arthritis, can cause a painful flatfoot. This type of arthritis attacks not only the cartilage in the joints, but also the ligaments that support the foot. Inflammatory arthritis not only causes pain, but also causes the foot to change shape and become flat. The arthritis can affect the back of the foot or the middle of foot, both of which can result in a fallen arch. An injury to the tendons or ligaments in the foot can cause the joints to fall out of alignment. The ligaments support the bones and prevent them from moving. If the ligaments are torn, the foot will become flat and painful. This more commonly occurs in the middle of the foot (Lisfranc injury), but can also occur in the back of the foot. Injuries to tendons of the foot can occur either in one instance (traumatically) or with repeated use over time (overuse injury). Regardless of the cause, if tendon function is altered, the forces that are transmitted across joints in the foot are changed and this can lead to increased stress on joint cartilage and ligaments. In addition to tendon and ligament injuries, fractures and dislocations of the bones in the midfoot can also lead to a flatfoot deformity. People with diabetes or with nerve problems that limits normal feeling in the feet, can have collapse of the arch or of the entire foot. This type of arch collapse is typically more severe than that seen in patients with normal feeling in their feet. In addition to the ligaments not holding the bones in place, the bones themselves can sometimes fracture and disintegrate without the patient feeling any pain. This may result in a severely deformed foot that is very challenging to correct with surgery. Special shoes or braces are the best method for dealing with this problem.
Symptoms
Some symptoms of adult acquired flat foot are pain along the inside of the foot and ankle, pain that increases with activity, and difficulty walking for long periods of time. You may experience difficulty standing, pain on the outside of the ankle, and bony bumps on the top of the foot and inside the foot. You may also have numbness and tingling of the feet and toes (may result from large bone spurs putting pressure on nerves), swelling, a large bump on the sole of the foot and/or an ulcer (in diabetic patients). Diabetic patients should wear a properly fitting diabetic shoe wear to prevent these complications from happening.
Diagnosis
Clinicians need to recognize the early stage of this syndrome which includes pain, swelling, tendonitis and disability. The musculoskeletal portion of the clinical exam can help determine the stage of the disease. It is important to palpate the posterior tibial tendon and test its muscle strength. This is tested by asking patient to plantarflex and invert the foot. Joint range of motion is should be assessed as well. Stiffness of the joints may indicate longstanding disease causing a rigid deformity. A weightbearing examination should be performed as well. A complete absence of the medial longitudinal arch is often seen. In later stages the head of the talus bone projects outward to the point of a large "lump" in the arch. Observing the patient's feet from behind shows a significant valgus rotation of the heel. From behind, the "too many toes" sign may be seen as well. This is when there is abducution of the forefoot in the transverse plane allowing the toes to be seen from behind. Dysfunction of the posterior tibial tendon can be assessed by asking the patient to stand on his/her toes on the affected foot. If they are unable to, this indicates the disease is in a more advanced stage with the tendon possibly completely ruptured.
Non surgical Treatment
It is imperative that you seek treatment should you notice any symptoms of a falling arch or PTTD. Due to the progressive nature of this condition, your foot will have a much higher chance of staying strong and healthy with early treatment. When pain first appears, your doctor will evaluate your foot to confirm a flatfoot diagnosis and begin an appropriate treatment plan. This may involve rest, anti-inflammatory medications, shoe modifications, physical therapy, orthotics and a possible boot or brace. When treatment can be applied at the beginning, symptoms can most often be resolved without the need for surgery.
Surgical Treatment
If initial conservative therapy of posterior tibial tendon insufficiency fails, surgical treatment is considered. Operative treatment of stage 1 disease involves release of the tendon sheath, tenosynovectomy, debridement of the tendon with excision of flap tears, and repair of longitudinal tears. A short-leg walking cast is worn for 3 weeks postoperatively. Teasdall and Johnson reported complete relief of pain in 74% of 14 patients undergoing this treatment regimen for stage 1 disease. Surgical debridement of tenosynovitis in early stages is believed to possibly prevent progression of disease to later stages of dysfunction.
Precisely What Can Cause Tendinitis Ache Of The Achilles ?
 The Achilles tendon is the largest tendon in the body. It connects the calf muscles to the heel and is active during almost all activities including walking, jumping, and swimming. This dense tendon can withstand large forces, but can become inflamed and painful during periods of overuse. Pain results from inflammation (tendonitis) or a degenerating tendon (tendinosis). Achilles tendon pathologies include rupture and tendonitis. Many experts now believe, however, that tendonitis is a misleading term that should no longer be used, because signs of true inflammation are almost never present on histologic examination. Instead, the following histopathologically determined nomenclature has evolved. Paratenonitis: Characterized by paratenon inflammation and thickening, as well as fibrin adhesions. Tendinosis: Characterized by intrasubstance disarray and degeneration of the tendon.
The Achilles tendon is the largest tendon in the body. It connects the calf muscles to the heel and is active during almost all activities including walking, jumping, and swimming. This dense tendon can withstand large forces, but can become inflamed and painful during periods of overuse. Pain results from inflammation (tendonitis) or a degenerating tendon (tendinosis). Achilles tendon pathologies include rupture and tendonitis. Many experts now believe, however, that tendonitis is a misleading term that should no longer be used, because signs of true inflammation are almost never present on histologic examination. Instead, the following histopathologically determined nomenclature has evolved. Paratenonitis: Characterized by paratenon inflammation and thickening, as well as fibrin adhesions. Tendinosis: Characterized by intrasubstance disarray and degeneration of the tendon.
Causes
Achilles tendinitis is typically not related to a specific injury. The problem results from repetitive stress to the tendon. This often happens when we push our bodies to do too much, too soon, but other factors can make it more likely to develop tendinitis, including a bone spur that has developed where the tendon attaches to the heel bone, Sudden increase in the amount or intensity of exercise activity-for example, increasing the distance you run every day by a few miles without giving your body a chance to adjust to the new distance, Tight calf muscles, Having tight calf muscles and suddenly starting an aggressive exercise program can put extra stress on the Achilles tendon, Bone spur-Extra bone growth where the Achilles tendon attaches to the heel bone can rub against the tendon and cause pain.
Symptoms
The most common site of Achilles Tendonitis is at the heel to 4 inches above the heel. The diagnosis of this problem is made when the following signs are present. Pain in the Achilles tendon with up and down movement of the foot at the ankle. Pain in the Achilles tendon when you squeeze the tendon from side to side. If you are unable to move the foot either up or down, or you have intense pain when trying to walk, you may have a tear of the Achilles tendon, and you should see a doctor immediately. Also if you have severe pain in the calf, with or without discolorations of the skin, you may have a blood clot, and this is a medical emergency; see a doctor immediately. If you do not fall into either of these categories then try the following suggestions.
Diagnosis
The doctor will perform a physical exam. The doctor will look for tenderness along the tendon and pain in the area of the tendon when you stand on your toes. X-rays can help diagnose bone problems. An MRI scan may be done if your doctor is thinking about surgery or is worried about the tear in the Achilles tendon.
Nonsurgical Treatment
In order to treat the symptoms, antiflogistics or other anti-inflammatory therapy are often used. However these forms of therapy usually cannot prevent the injury to live on. Nevertheless patients will always have to be encouraged to execute less burdening activities, so that the burden on the tendon decreases as well. Complete immobilisation should however be avoided, since it can cause atrophy. Passive rehabilitation, Mobilisations can be used for dorsiflexion limitation of the talocrural joint and varus- or valgus limitation of the subtalar joint. Deep cross frictions (15 min). It?s effectiveness is not scientifically proven and gives limited results. Recently, the use of Extracorporal Shock Wave Therapy was proven. Besides that, the application of ice can cause a short decrease in pain and in swelling. Even though cryotherapy 2, 5 was not studied very thoroughly, recent research has shown that for injuries of soft tissue, applications of ice through a wet towel for ten minutes are the most effective measures. Active rehabilitation, An active exercise program mostly includes eccentric exercises. This can be explained by the fact that eccentric muscle training will lengthen the muscle fibres, which stimulates the collagen production. This form of therapy appears successful for mid-portion tendinosis, but has less effect with insertion tendinopathy. The sensation of pain sets the beginning burdening of the patient and the progression of the exercises.

Surgical Treatment
Surgery should be considered to relieve Achilles tendinitis only if the pain does not improve after 6 months of nonsurgical treatment. The specific type of surgery depends on the location of the tendinitis and the amount of damage to the tendon. Gastrocnemius recession. This is a surgical lengthening of the calf (gastrocnemius) muscles. Because tight calf muscles place increased stress on the Achilles tendon, this procedure is useful for patients who still have difficulty flexing their feet, despite consistent stretching. In gastrocnemius recession, one of the two muscles that make up the calf is lengthened to increase the motion of the ankle. The procedure can be performed with a traditional, open incision or with a smaller incision and an endoscope-an instrument that contains a small camera. Your doctor will discuss the procedure that best meets your needs. Complication rates for gastrocnemius recession are low, but can include nerve damage. Gastrocnemius recession can be performed with or without d?bridement, which is removal of damaged tissue. D?bridement and repair (tendon has less than 50% damage). The goal of this operation is to remove the damaged part of the Achilles tendon. Once the unhealthy portion of the tendon has been removed, the remaining tendon is repaired with sutures, or stitches to complete the repair. In insertional tendinitis, the bone spur is also removed. Repair of the tendon in these instances may require the use of metal or plastic anchors to help hold the Achilles tendon to the heel bone, where it attaches. After d?bridement and repair, most patients are allowed to walk in a removable boot or cast within 2 weeks, although this period depends upon the amount of damage to the tendon. D?bridement with tendon transfer (tendon has greater than 50% damage). In cases where more than 50% of the Achilles tendon is not healthy and requires removal, the remaining portion of the tendon is not strong enough to function alone. To prevent the remaining tendon from rupturing with activity, an Achilles tendon transfer is performed. The tendon that helps the big toe point down is moved to the heel bone to add strength to the damaged tendon. Although this sounds severe, the big toe will still be able to move, and most patients will not notice a change in the way they walk or run. Depending on the extent of damage to the tendon, some patients may not be able to return to competitive sports or running. Recovery. Most patients have good results from surgery. The main factor in surgical recovery is the amount of damage to the tendon. The greater the amount of tendon involved, the longer the recovery period, and the less likely a patient will be able to return to sports activity. Physical therapy is an important part of recovery. Many patients require 12 months of rehabilitation before they are pain-free.
Prevention
There are several things you can do to reduce the risk of Achilles tendinitis, warm up every time before you exercise or play a sport. Switch up your exercises. Slowly increase the length and intensity of your workouts. Keep your muscles active and stay in shape all year-round. When you see symptoms of Achilles tendinitis, stop whatever activity you are doing and rest.
What Is Heel Discomfort

Overview
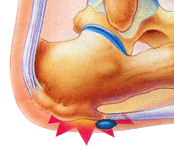
Plantar fasciitis refers to an inflammation of the plantar fascia, a thick, fibrous band running along the sole of the foot. Such inflammation results from direct injury to the plantar fascia, usually, repeated trauma to the tissue where the fascia attaches to the calcaneus or heel bone. The plantar fascia is critical in maintaining the foot’s complex arch system, also playing a role in balance and fine control of certain phases of the athlete’s gait. Injury to the plantar fascia is particularly painful and disabling for runners and can often prove stubbornly resistant to treatment. Rehabilitation is frequently a lengthy and frustrating process. For these reasons, care should be taken where possible to avoid such injury by means of preventative exercises and sensitivity to early warning signs.
Causes
Under normal circumstances, your plantar fascia acts like a shock-absorbing bowstring, supporting the arch in your foot. If tension on that bowstring becomes too great, it can create small tears in the fascia. Repetitive stretching and tearing can cause the fascia to become irritated or inflamed.
Symptoms
Plantar fasciosis is characterized by pain at the bottom of the heel with weight bearing, particularly when first arising in the morning; pain usually abates within 5 to 10 min, only to return later in the day. It is often worse when pushing off of the heel (the propulsive phase of gait) and after periods of rest. Acute, severe heel pain, especially with mild local puffiness, may indicate an acute fascial tear. Some patients describe burning or sticking pain along the plantar medial border of the foot when walking.
Diagnosis
Plantar fasciosis is confirmed if firm thumb pressure applied to the calcaneus when the foot is dorsiflexed elicits pain. Fascial pain along the plantar medial border of the fascia may also be present. If findings are equivocal, demonstration of a heel spur on x-ray may support the diagnosis; however, absence does not rule out the diagnosis, and visible spurs are not generally the cause of symptoms. Also, infrequently, calcaneal spurs appear ill defined on x-ray, exhibiting fluffy new bone formation, suggesting spondyloarthropathy (eg, ankylosing spondylitis, reactive arthritis. If an acute fascial tear is suspected, MRI is done.
Non Surgical Treatment
No single treatment works best for everyone with plantar fasciitis. But there are many things you can try to help your foot get better. Give your feet a rest. Cut back on activities that make your foot hurt. Try not to walk or run on hard surfaces. To reduce pain and swelling, try putting ice on your heel. Or take an over-the-counter pain reliever like ibuprofen (such as Advil or Motrin) or naproxen (such as Aleve). Do toe stretches , calf stretches and towel stretches several times a day, especially when you first get up in the morning. (For towel stretches, you pull on both ends of a rolled towel that you place under the ball of your foot.) Get a new pair of shoes. Pick shoes with good arch support and a cushioned sole. Or try heel cups or shoe inserts ( orthotics ). Use them in both shoes, even if only one foot hurts. If these treatments do not help, your doctor may recommend splints that you wear at night, shots of medicine (such as a steroid ) in your heel, or other treatments. You probably will not need surgery. Doctors only suggest it for people who still have pain after trying other treatments for 6 to 12 months.

Surgical Treatment
Most studies indicate that 95% of those afflicted with plantar fasciitis are able to relieve their heel pain with nonsurgical treatments. If you are one of the few people whose symptoms don't improve with other treatments, your doctor may recommend plantar fascia release surgery. Plantar fascia release involves cutting part of the plantar fascia ligament in order to release the tension and relieve the inflammation of the ligament. Overall, the success rate of surgical release is 70 to 90 percent in patients with plantar fasciitis. While the success rate is very high following surgery, one should be aware that there is often a prolonged postoperative period of discomfort similar to the discomfort experienced prior to surgery. This pain usually will abate within 2-3 months. One should always be sure to understand all the risks associated with any surgery they are considering.
What Brings About Plantar Fasciitis To Flare Up

Overview
Plantar fasciitis is a common painful disorder affecting the heel and underside of the foot. It is a disorder of the insertion site of plantar fascia on the bone and is characterized by scarring, inflammation, or structural breakdown of the foot’s plantar fascia. It is often caused by overuse injury of the plantar fascia, increases in exercise, weight or age. Although plantar fasciitis was originally thought to be an inflammatory process, newer studies have demonstrated structural changes more consistent with a degenerative process. As a result of this new observation, many in the academic community have stated the condition should be renamed plantar fasciosis.
Causes
It is common to see patients with Plantar Fasciitis who have been wearing shoes that are too soft and flexible. The lack of support can be stressful on the heel for those patients who’s feet aren’t particularly stable. If these ill fitting shoes are worn for long enough, the stress will lead to Heel Pain as the inflammation of the fascia persists. Footwear assessment and advice will be essential in order to get on top of the Plantar Fasciitis. It may surprise some people to learn that high heeled shoes are not the cause of Plantar Fasciitis, although they can cause tight calf muscles. High arches can lead to Plantar Fasciitis. This is due to the lack of contact under the sole of the foot. Even sports shoes which appear to have good arch support inside are often too soft and not high enough to make contact with the arch of the foot. Hence, the plantar fascia is unsupported. This can lead to Heel pain and Plantar Fasciitis. Flat feet can lead to Plantar Fasciitis. Flat feet is caused by ligament laxity and leads to foot instability. Other structures such as muscles, tendons and fascia work harder to compensate for this instability. Heel pain or Plantar Fasciitis arises when the instability is too great for these other structures to cope with. The strain on the fascia is too severe and the inflammation sets in. Over stretching can lead to Plantar Fasciitis. Certain calf stretches put the foot into a position that creates a pulling sensation through the sole of the foot. This can cause Plantar Fasciitis which can cause pain in the arch of the foot as well as Heel Pain.
Symptoms
Plantar fasciitis typically causes a stabbing pain in the bottom of your foot near the heel. The pain is usually worst with the first few steps after awakening, although it can also be triggered by long periods of standing or getting up from a seated position.
Diagnosis
Plantar fasciitis is usually diagnosed by a health care provider after consideration of a person’s presenting history, risk factors, and clinical examination. Tenderness to palpation along the inner aspect of the heel bone on the sole of the foot may be elicited during the physical examination. The foot may have limited dorsiflexion due to tightness of the calf muscles or the Achilles tendon. Dorsiflexion of the foot may elicit the pain due to stretching of the plantar fascia with this motion. Diagnostic imaging studies are not usually needed to diagnose plantar fasciitis. However, in certain cases a physician may decide imaging studies (such as X-rays, diagnostic ultrasound or MRI) are warranted to rule out other serious causes of foot pain. Bilateral heel pain or heel pain in the context of a systemic illness may indicate a need for a more in-depth diagnostic investigation. Lateral view x-rays of the ankle are the recommended first-line imaging modality to assess for other causes of heel pain such as stress fractures or bone spur development. Plantar fascia aponeurosis thickening at the heel greater than 5 millimeters as demonstrated by ultrasound is consistent with a diagnosis of plantar fasciitis. An incidental finding associated with this condition is a heel spur, a small bony calcification on the calcaneus (heel bone), which can be found in up to 50% of those with plantar fasciitis. In such cases, it is the underlying plantar fasciitis that produces the heel pain, and not the spur itself. The condition is responsible for the creation of the spur though the clinical significance of heel spurs in plantar fasciitis remains unclear.
Non Surgical Treatment
Treatment initially involves offloading the plantar fascia by aoiding aggravating factors, such as running. Taping, this can work very well to alleviate pain, and can be almost immediate. It isn't a long-term solution, but can relieve symptoms in the beginning. Using a night splint to stretch the calf, so that less load is placed on the plantar fascia (if tightness in the calf is a factor). Using a gel heel cup, this can act to increase shock absorption, and by raising the heel there is also less stretch on the calf. So, temporarily, this may relieve pain in someone who has a tight calf. Massage, but this depends if the plantarfascia is actually tight or just painful. If it is tight, then massage can temporarily relieve the pain, but if it is irritated then taping and corrective footwear is preferable.

Surgical Treatment
The most common surgical procedure for plantar fasciitis is plantar fascia release. It involves surgical removal of a part from the plantar fascia ligament which will relieve the inflammation and reduce the tension. Plantar fascia release is either an open surgery or endoscopic surgery (insertion of special surgical instruments through small incisions). While both methods are performed under local anesthesia the open procedure may take more time to recover. Other surgical procedures can be used as well but they are rarely an option. Complications of plantar fasciitis surgery are rare but they are not impossible. All types of plantar fasciitis surgery pose a risk of infection, nerve damage, and anesthesia related complications including systemic toxicity, and persistence or worsening of heel pain.
Prevention
While there are no sure ways to prevent plantar fasciitis, these prevention tips may be helpful. Keep your weight under reasonable control. Wear comfortable, supportive shoes. Use care when starting or intensifying exercise programmes.